Pelvic Venous Congestion
Varicose veins can also develop in the pelvis and this can cause disabling symptoms in women of the child bearing age group. This is known as Pelvic Venous Congestion.
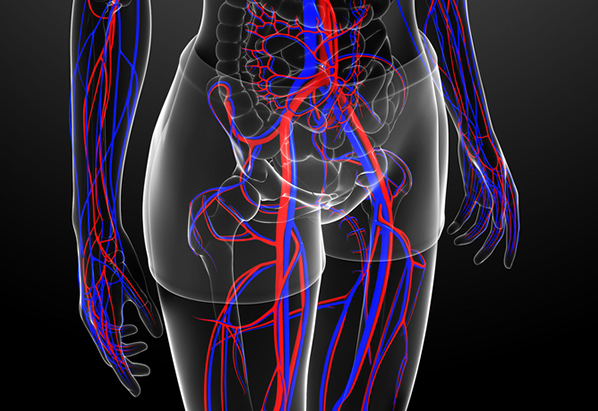 Figure showing complex network of pelvic veins
Figure showing complex network of pelvic veinsWhat causes Pelvic venous congestion?
Pelvic varicose veins can be caused due to
- Incompetent pelvic veins which are unable to drain blood efficiently and this may be related to hormonal factors in women.
- Obstruction to the normal venous blood flow due to conditions such as May Thurner syndrome and Nutcracker syndrome can lead to the formation of alternate venous channels which can become varicose.
- Other pelvic conditions such as endometriosis or tumours can also cause PVC.
What are the symptoms of Pelvic Venous Congestion?
- Pain in the pelvic area is one of the most common symptoms. It is often described as a dull ache or throb
- Pain worse during or after sex, during menstruation and after prolonged standing.
- Varicose veins maybe noted in the vagina, the upper thigh, along the buttocks and legs.
How is it diagnosed?
Pelvic venous congestion is difficult to diagnose. First and foremost, it is important to exclude other pelvic causes for these symptoms. Often, a referral to a vascular surgeon is made by an Obstetrics and Gynaecology specialist who has excluded other causes for these symptoms. Some investigations that may help with the diagnosis are
- Pelvic ultrasound scan
- CT and MR venography and
- Selective venography
What are the treatment options?
There are various options available for the treatment of Pelvic venous congestion However, endovascular treatment which is a keyhole treatment is the most popular one.
-

Endovascular Treatment
- This is the commonest and most effective treatment option available for Pelvic venous congestion. The procedure is performed under a local anaesthetic. A catheter (narrow tube) is introduced over a sheath (plastic sleeve) via the femoral vein in the groin. The catheter is then manipulated and directed within the lumen of the veins to identify incompetent (faulty) veins using contrast (dye) venography. These veins are then permanently blocked using fine metal coils or plugs and medical grade foam and glue.

Medical Treatment
- Some patients note improvement in their symptoms after treatment with hormone replacement therapy although this response may not be long lasting.

Laparoscopic Surgery
- This invasive treatment option involves surgery under a general anaesthetic to tie off the faulty veins.