Chronic Venous Ulcers (Chronic Venous Insufficiency)
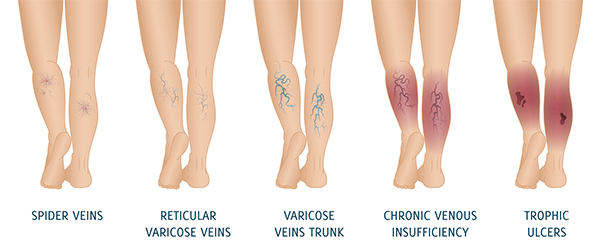
Chronic venous ulcers are a consequence of Chronic venous insufficiency (CVI) and both these are covered in this section. CVI is a condition where the veins are incompetent due to faulty valves and unable to return blood effectively from the lower limbs back to the heart. This causes blood to pool or collect in the veins and this is called stasis. This stasis can consequently result in increased back pressure in the smaller veins and tissues that lead to changes over the lower leg. These include early changes such as swelling, dermatitis, eczema and darkening of skin and then chronic venous ulcerations (sores).
What are the risk factors for Chronic venous insufficiency /ulcers?
Risk factors make you a more likely candidate to develop CVI. Some of the important risk factors for CVI and Chronic venous ulcers are
- Deep vein thrombosis
- Varicose veins and a family history of varicose veins
- Obesity and inactivity
What are the symptoms of CVI?
Most symptoms of CVI are mild and do not pose any risk to the limb. Some of the commonly described symptoms of CVI are
- Heaviness and tiredness of the affected leg.
- Swelling in the legs especially after standing for some duration.
- Darkening of the skin above the ankle (hyperpigmentation),
- Dermatitis, eczema and thickening of the skin which appears shiny (Lipodermatosclerosis)
- Open sores or ulcers (usually on the inside of the ankle)
- Prominent varicose veins (enlarged and twisted veins) just under the skin and may experience burning and pain.
How is CVI diagnosed?
In addition to physical examination, your doctor will recommend a
- Duplex ultrasound imaging to detect faulty or incompetent veins and also for evidence of previous deep vein thrombosis (clots).
- CT scan may sometimes help to determine if the larger veins are narrowed or blocked.
What are the treatment options?
The main aim of treatment for CVI is to prevent severe swelling and ulcers from developing.
-

Compression Stockings
- Compression stockings are designed to help reduce the swelling in the legs following DVT and it also improves the drainage of blood from the legs.
-

Sclerotherapy
- This involves injecting a medical grade irritant into the lumen of the varicose vein. This in turn causes inflammation of the varicose vein which subsequently scars up. You may require multiple injections on separate sittings to treat all the varicose veins but the procedure is done under a local anaesthetic.
-

Angioplasty and Stenting
- Angioplasty and stenting will be rarely recommended in cases where the larger veins in the abdomen (iliac veins or IVC) are narrowed or blocked. This keyhole procedure uses a small balloon to stretch the narrowed vein and the stent (metal mesh) prevents further narrowing of the vein in the future.
Varicose veins can be treated by ablation, vein stripping or sclerotherapy
Management of Chronic Venous Ulcers
This can be very challenging and it often takes considerable time (months) before some improvement is seen. Some of the treatment strategies to help ulcer healing are
- Regular inspection and cleaning of ulcers and appropriate dressing changes by an expert in ulcer care and management
- Treating infections promptly with antibiotics
- Leg elevation whilst in bed to reduce the swelling in the legs
- Compression bandaging to improve venous blood return and reduce leg swelling
- Treatment of the varicose veins may also help prevent recurrence of ulcers in the future.
Can CVI and ulcers be prevented?
CVI can worsen and progress if left untreated and hence it is important to
- Maintain good skin care
- Wear compression stockings as advised.
- Anticoagulation medications - individuals with deep vein thrombosis should adhere to the anticoagulation medications strictly.
- Maintaining a normal weight and regular exercise can also make a difference and keep the symptoms of CVI under control.